The increasing utilization of private healthcare for medical exams and procedures is adding strain to already overburdened GP practices. Family physicians are cautioning that the availability of standard NHS services is being reduced as a consequence.
An increasing number of individuals are choosing to pay for their own healthcare, including procedures like cataract surgery and hip replacements. This is due to growing dissatisfaction with lengthy waiting lists at NHS hospitals. Additionally, some are selecting private health screenings, genetic testing, or cosmetic surgeries like liposuction.
The rise in private healthcare utilization is adding to the responsibilities of GPs, who report having to decipher potentially unreliable private health screenings, coordinate laboratory tests and imaging, and handle extra administrative tasks associated with private care. Some GPs also note that a larger portion of their time is now spent on follow-up appointments for patients who received treatment or surgery overseas.
A GP expressed concern that the NHS general practice is being taken advantage of and financially supporting profitable private practices that charge excessive fees to patients. Another physician stated that addressing dubious medical requests from private healthcare providers, which they do not approve of clinically, is consuming valuable time and resources that could be used for standard NHS patients.
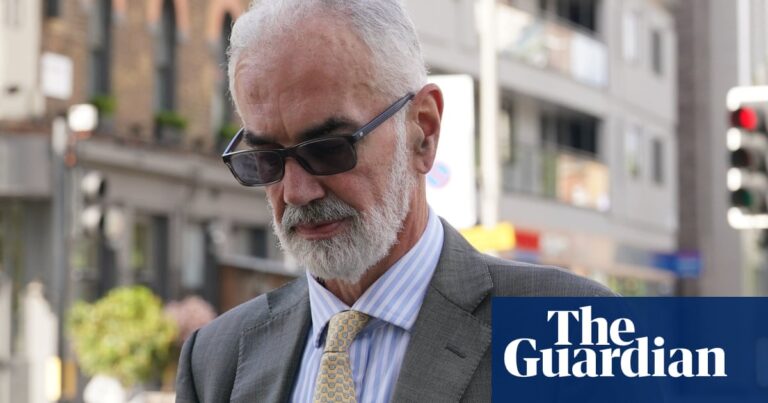
Dr John Puntis, the co-chair of the Keep Our NHS Public campaign group, said: “This is a sorry picture not only of hard-pressed GPs having their workloads and stress levels unnecessarily increased, but also patients duped by the private sector into paying out cash for sometimes dubious tests, diagnoses and procedures without adequate provision for follow-up advice and care.”
A survey conducted by Pulse, a magazine for family doctors, and reviewed by the Guardian found that nearly half of GPs have experienced an increase in workload due to the use of private healthcare.
According to a survey of 860 general practitioners, 46% of family doctors have noted an increase in their workload due to the rise in private healthcare utilization. Additionally, 10% stated that their workload has significantly risen as a result.
According to Dr Emma Nash, a general practitioner in Portchester, Hampshire, she has noticed a significant rise in her workload due to private healthcare.
“Initially, it adds to our administrative tasks, such as requesting and reviewing blood tests and communicating results, as well as spending time reading lengthy reports. This is in addition to our already heavy workload.”
“The most aggravating aspect is when we are presented with reports or requests that we do not concur with clinically or do not comprehend the reasoning behind. This ultimately leads to NHS patients losing their appointments because once we have been informed, we cannot undo the knowledge.”
Nash explained that this primarily pertains to situations where an individual has numerous tests conducted by a private healthcare company, and then relies on GPs to communicate the findings to the patient.
Some of the time is used for consultations that were recommended by a private clinician. In some cases, this is not necessary because the patient does not meet the requirements, while other times it could have been handled by the private clinician. This type of consultation can be difficult and could have been avoided.
Nash stated that requesting tests involves more than simply checking off boxes. They also have a legal obligation to review, interpret, and respond to the results, which can be a time-consuming process.
She stated: “While it is not mandatory for us to conduct these tests or provide prescriptions, it can be challenging when a patient has already been informed about what to expect. The NHS is responsible for addressing the outcomes of private work, regardless of its appropriateness.”
“Although not all elements of this provision result in a loss of time for standard NHS care, many do. Additionally, the psychological strain of this workload is significant – we are already overwhelmed by our own work, which is generated by the NHS. This is a growing issue that is negatively affecting morale and contributing to burnout.”
According to Dr. David Coleman, a general practitioner in Doncaster, the practice is currently experiencing an increase in workload due to private inquiries about ADHD, resulting in a couple of extra hours of work each week.
Dr. Zishan Syed, a general practitioner in Kent, expressed that the National Health Service’s general practice is being taken advantage of and supporting profitable private practices that are overcharging patients. This puts pressure on GPs to handle complex administrative tasks for free, which is absurd and undermines the integrity of the NHS and the taxpayers.
Syed expressed that the current guidelines regarding the interaction between private and NHS sectors were comical. Nash also stated that the regulations were inadequate.
According to Cat Hobbs, the leader of We Own It, a public-ownership campaign group, it is crucial for the government to restore the NHS as a fully public service and provide adequate funding. Otherwise, there is a risk of transitioning into a costly, American-style system with two tiers where GPs are unable to manage the workload.
Prof Kamila Hawthorne, chair of the Royal College of GPs, warned the UK must “guard against creating a two-tier system that favours those who can afford to pay and disadvantages those who can’t” but said she understood why some patients facing NHS waits turn to private healthcare.
According to the speaker, numerous private clinics transfer their findings to the NHS, typically through general practitioners, for evaluation and continued monitoring. In addition, some private companies regularly suggest that their clients consult with their NHS GP regarding their results or treatment, even if everything has been successful. This can contribute to increased workload for GPs and result in longer wait times for other patients seeking appointments.
Source: theguardian.com