Women could be offered DIY cervical screening tests on the NHS, after research found self-testing at home significantly improved screening rates.
Researchers calculated that being able to take their sample at home could encourage about 400,000 more women a year to have a cervical screening.
Cervical cancer is the 14th most common cancer affecting women in Britain. About 13 high-risk types of human papillomavirus (HPV) are known to cause 99.7% of all cervical cancers. About 3,200 women in the UK are diagnosed with cervical cancer every year, of whom 850 die from it.
Amanda Pritchard, the head of NHS England, has pledged to eliminate cervical cancer by 2040 through screening and vaccination.
The HPV vaccination programme was introduced in 2008 in England and since 2019 is given to boys as well as girls aged 12 and 13. The NHS encourages women to have a cervical screening every three to five years, even if they are vaccinated, as the jab does not protect against all forms of HPV.
But the latest figures show cervical screening attendance is declining, with nearly a third of women in England – particularly younger women, those from minority ethnic backgrounds and deprived areas – not taking up their most recent test.
Women might choose not to go to a screening because of embarrassment, worries it will hurt and lack of convenient appointments.
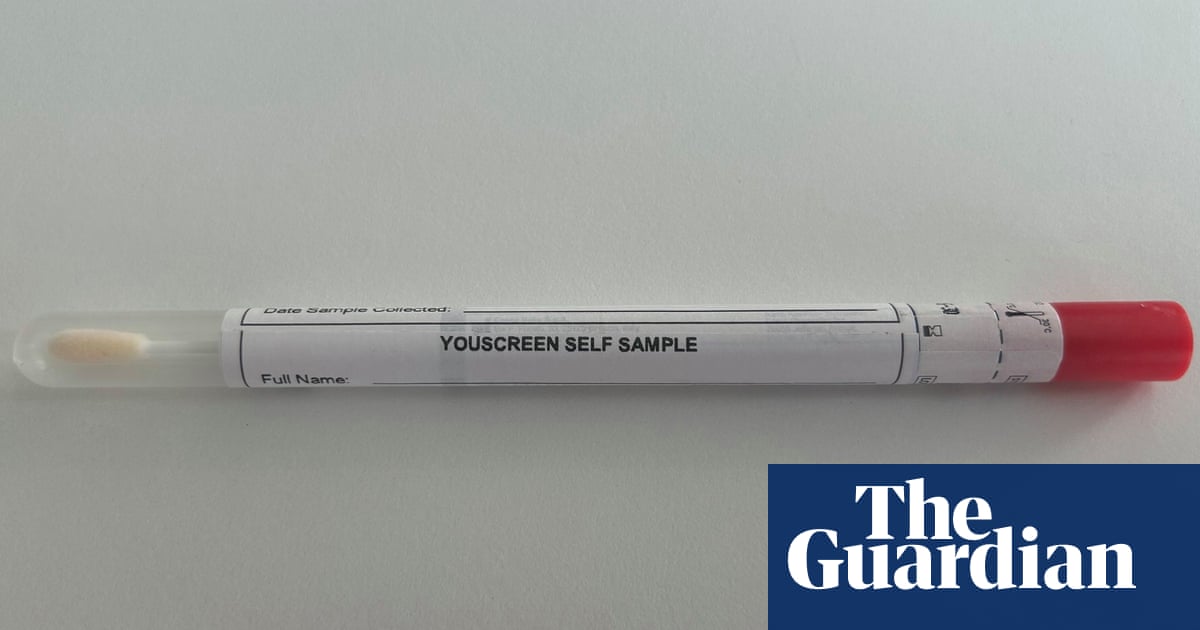
Academics at King’s College London conducted the biggest trial of self-sampling in the UK to date. Published in the journal eClinicalMedicine, the trial studied 27,000 women who were at least six months overdue for their cervical screening and found that DIY kits, especially those directly given to women by their GP surgery, could significantly increase their uptake of the screening.
“Self-sampling has been hailed as a gamechanger for cervical screening and we now have evidence in a UK population to show that it really is,” said Dr Anita Lim, the lead author of the study and a senior research fellow at King’s College London.
“It’s really encouraging that we received self-samples from groups that have been historically underserved including people from deprived and ethnic minority backgrounds, LGBTQI+, people with learning disabilities and victims of sexual violence.”
Before home testing could be routinely offered by the health service, the UK National Screening Committee would need to evaluate the efficacy and assess the risk and extent of overdiagnosis.
NHS England’s director of screening and vaccination, Deborah Tomalin, said the NHS would assess whether self-sampling could be rolled out in England. “It’s extremely promising that this study suggests simple DIY swab tests could have a really positive impact in supporting more women to take part in cervical screening from their own homes, and the NHS will now be working with the UK National Screening Committee to consider the feasibility of rolling this out more widely across England,” she said.
In the trial, 17,604 vaginal swab kits were sent to women through the post, while 10,849 women were offered a kit when speaking to their GP surgery about something else.
The study found that 56% of those offered a DIY test at their GP surgery and 13% of those sent one through the post returned their screening test, while 52% of all those who returned a self-sample were at least two years overdue screening, including those who had never previously been screened.
after newsletter promotion
Sixty-four per cent were from minority ethnic groups and 60% from deprived populations.
The study calculated that expanding self-sampling in England could increase national screening coverage from 69.9% to 77.3%, which would lead to more than 1 million additional women being screened every three years in England.
Prof Peter Sasieni, the head of the research group at King’s College London and now at Queen Mary University of London, said the UK was “well on the way to turning cervical cancer into a rare disease”.
He said while the HPV jab in schools was offering huge benefit, women born before 1990 still needed regular screening as they had not been vaccinated against cervical cancer.
Responding to the findings, Sophia Lowes, Cancer Research UK’s senior health information manager, said self-sampling could help to address some of the barriers to cervical screening and in turn tackle health inequalities.
“If coverage of cervical screening and HPV vaccination increases, it’s possible that we can reduce cervical cancer to the point where almost no one develops it,” she added. “Further research is now needed to better understand the accuracy of self-sampling and how it can be effectively rolled out to benefit more people.”
Source: theguardian.com


















